Drug & Food Allergy
Drug & Food Allergy
General Considerations
Some drugs are clearly more immunogenic than others, and
this can be reflected in the incidence of drug hypersensitivity. A partial list
of drugs frequently implicated in drug reactions includes B-lactam antibiotics,
sulfonamides, phenytoin, carbamazepine, allopurinol, muscle relaxants used for
general anesthesia, nonsteroidal anti-inflammatory drugs, antisera, and
antiarrhythmic agents. Many drugs can be associated with recognizable known
toxicities, drug interactions, or idiosyncratic reactions that are not
immune-mediated. These must be distinguished from true hypersensitivity
reactions because the prognosis and management differ. Some estimate that only
10% or less of adverse reactions to drugs are true hypersensitivity reactions.
Patients with multidrug hypersensitivity are quite rare, and those reporting
"allergies" to more than three distinct classes of drugs should be carefully
evaluated since intolerance to many of these drug classes may not be
immunologic.
Four foods account for 90% of food allergy in adults:
peanuts, tree nuts, fish, and shellfish. Food hypersensitivity must be
distinguished from food intolerance, which is more common and more variable in
terms of underlying mechanism. An example of food intolerance would be lactose
intolerance, which is due to an enzyme deficiency rather than an IgE-mediated
hypersensitivity.
Clinical Findings of Drug & Food Allergy
Symptoms and Signs
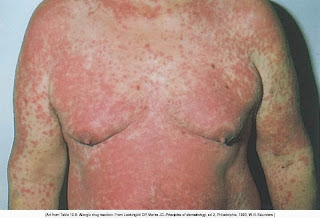
The development of symptoms and the nature of the adverse
drug reaction can suggest whether an immunologic process is responsible for
symptoms. Factors to consider include type of symptoms, history of previous drug
exposure, time of onset after starting the drug, presence of other systemic
involvement, coexisting illness, and concurrent drug use. In previously
sensitized individuals, immediate hypersensitivity is manifested by rapid
development of urticaria, angioedema, or anaphylaxis. Delayed onset of urticaria
accompanied by fever, arthralgias, and nephritis may indicate the development of
an immune complex-mediated disorder. Drug fever and Stevens-Johnson syndrome
probably act by immune hypersensitivity mechanisms. In genetically slow
acetylators and in AIDS patients with depleted hepatic glutathione levels, drugs
such as sulfamethoxazole are not rapidly excreted during drug metabolism. This
altered drug metabolism favors the generation of haptenated immunoreactive
metabolites as well as drug reactions, such as delayed morbilliform eruptions.
Other types of immune-mediated dermatologic drug reactions include lupus-like
syndromes caused by procainamide, isoniazid, phenytoin, or hydralazine. Drugs
that have been associated with the development of systemic or cutaneous
vasculitis include leukotriene receptor antagonists, allopurinol, phenytoin,
thiazides, nonsteroidal anti-inflammatory drugs, furosemide, cimetidine, gold,
hydralazine, and many antibiotics (eg, penicillin, sulfonamides, quinolones, and
tetracycline). Cutaneous vasculitides are usually associated with fixed lesions,
with histologically-proven immune-complex involvement.
Food hypersensitivity is manifest by symptoms
consistent with IgE-mediated immediate hypersensitivity/anaphylaxis but
commonly is also accompanied by abdominal pain, nausea, vomiting, or diarrhea.
More rarely, atopic dermatitis may be the sole clinical expression of
food allergy. The onset of allergic food reactions is rapid, usually within
minutes to a couple of hours of ingestion, and the reaction is usually quite
reproducible. Oral allergy syndrome is a self-limited form of fruit and
vegetable hypersensitivity, where symptoms are confined to the oropharynx. Due
to cross-reactivity between certain fruit and vegetable allergens and certain
seasonal pollens, ingestion of these foods causes a contact allergy with
pruritus of lips, tongue, and palate typically without other symptoms or signs
of systemic anaphylaxis. The most common cross-reacting foods and pollens are
apples and carrots, which cross-react with birch pollen; melons and bananas,
which cross-react with ragweed pollen. Many of these antigens involved in oral
allergy syndrome are heat labile and denature during cooking. Immunologic
cross-reactivity appears to also underlie the association of latex allergy and
hypersensitivity to avocado, banana, chestnut, kiwi, and papaya. Unlike the oral
allergy syndrome, however, systemic anaphylaxis upon ingestion of these foods
may develop in 35–50% of patients who are allergic to latex (so called
latex-fruit syndrome).
Laboratory Findings
Allergy testing
Allergy skin testing is only available for a limited number
of drugs (penicillin, insulin, streptokinase, chymopapain, heterologous serum),
since patients may react to the native drug as well as any metabolite that
covalently binds to native protein and becomes immunoreactive. Skin testing is
available for patients with suspected immediate hypersensitivity to penicillin
or  -lactam
antibiotics (see Infectious Diseases: Common Problems & Antimicrobial
Therapy). The degree of cross-reactivity between the cephalosporin antibiotics
and penicillins is uncertain. The incidence of IgE-mediated hypersensitivity
appears to be less than 5%. There appears to be no allergic cross-reactivity
between the monobactam antibiotics (aztreonam) and penicillin or other
-lactam
antibiotics (see Infectious Diseases: Common Problems & Antimicrobial
Therapy). The degree of cross-reactivity between the cephalosporin antibiotics
and penicillins is uncertain. The incidence of IgE-mediated hypersensitivity
appears to be less than 5%. There appears to be no allergic cross-reactivity
between the monobactam antibiotics (aztreonam) and penicillin or other  -lactam
antibiotics. A high degree of cross-reactivity exists between penicillin and the
carbapenem, imipenem, so this drug should be given to the penicillin-allergic
patient with the same degree of caution as if the patient were to receive
penicillin.
-lactam
antibiotics. A high degree of cross-reactivity exists between penicillin and the
carbapenem, imipenem, so this drug should be given to the penicillin-allergic
patient with the same degree of caution as if the patient were to receive
penicillin.
 -lactam
antibiotics (see Infectious Diseases: Common Problems & Antimicrobial
Therapy). The degree of cross-reactivity between the cephalosporin antibiotics
and penicillins is uncertain. The incidence of IgE-mediated hypersensitivity
appears to be less than 5%. There appears to be no allergic cross-reactivity
between the monobactam antibiotics (aztreonam) and penicillin or other
-lactam
antibiotics (see Infectious Diseases: Common Problems & Antimicrobial
Therapy). The degree of cross-reactivity between the cephalosporin antibiotics
and penicillins is uncertain. The incidence of IgE-mediated hypersensitivity
appears to be less than 5%. There appears to be no allergic cross-reactivity
between the monobactam antibiotics (aztreonam) and penicillin or other  -lactam
antibiotics. A high degree of cross-reactivity exists between penicillin and the
carbapenem, imipenem, so this drug should be given to the penicillin-allergic
patient with the same degree of caution as if the patient were to receive
penicillin.
-lactam
antibiotics. A high degree of cross-reactivity exists between penicillin and the
carbapenem, imipenem, so this drug should be given to the penicillin-allergic
patient with the same degree of caution as if the patient were to receive
penicillin.
If the likelihood of immunologic reaction is low—based on
the history and the assessment of likely offending agents—and if no allergy
testing is available, judicious test dose challenges may be considered in a
monitored setting. If the likelihood of IgE-mediated reaction is significant,
these challenges are risky and rapid drug desensitization is indicated.
The gold standard for allergy food testing is skin-prick
testing with actual food items, but due to the inconvenience and potential risk
for systemic reactions, this form of testing is usually preceded by IgE RAST
testing or skin prick testing with commercially available extracts or both. Food
allergy testing must be interpreted within the context of the clinical picture,
since false-positive tests can occur.
Provocation tests
Occasionally, direct allergen challenge of the target organ
or tissue under controlled conditions is required for definitive diagnosis. Such
challenges may be bronchial, nasal, conjunctival, oral, or cutaneous. A positive
test confirms that the test substance can cause the reaction, but it does not
prove that an immunologic mechanism is responsible.
In most cases of suspected allergy to a food or drug,
placebo-controlled oral challenge is the definitive test. To be considered a
positive result, the reported clinical findings must be reproduced during
provocation testing. A blinded provocation test may be preceded by an open
challenge (no placebo control), which, if negative, negates the necessity for
logistically difficult blinded challenge. Freeze-dried foods in large opaque
capsules provide a sufficient dose of allergen for testing. This should not be
done in patients with suspected food- or drug-induced anaphylaxis.
Treatment
For IgE-mediated drug hypersensitivity, acute rapid
desensitization may allow administration of a drug if there is no suitable
alternative treatment regimen. This procedure carries a significant risk and
should be undertaken in an intensively monitored setting. This is accomplished
by a course of oral or parenteral doses starting with extremely low doses
(dilutions of 1 x 10–6 or 1 x
10–5 units) and increasing to the full dose over a period of hours.
IgE-mediated reactivity diminishes during the course of this desensitization,
creating a temporary drug-specific refractory state. During the refractory
period, skin histamine responsiveness is maintained, and mast cells may be
activated by other stimuli but the patient may receive the desired drug with a
very low risk of anaphylaxis. Acute rapid desensitization may work through
cellular mechanisms different from those involved in standard injection
immunotherapy, and the refractory period is maintained only throughout the
course of uninterrupted therapy.
Various slow desensitization protocols have been developed
for patients suffering from late-appearing morbilliform eruptions (eg, AIDS
patients with sulfamethoxazole-induced dermatitis). These eruptions are not
IgE-mediated, and the slow reintroduction of drug allows for less haptenation
during sulfonamide metabolism with generation of less immunoreactive drug
metabolites. This form of desensitization is distinct from rapid desensitization
of IgE-mediated drug allergy. Desensitization for non–IgE-mediated drug
reactions has been successful for aspirin, nonsteroidal anti-inflammatory drugs,
and allopurinol.
Any history or finding consistent with toxic epidermal
necrolysis or Stevens-Johnson syndrome would be an absolute contraindication for
drug readministration.
For any proven food hypersensitivity, strict avoidance is
the only rational recommendation. Patients should also be provided with an
epinephrine autoinjector (Epi-pen) if indicated.
I hope, Drug & Food Allergy article be usefull for your.
Recources:
Current Medical Diagnosis & Treatment 2008
Stephen J. McPhee, Maxine A. Papadakis, and Lawrence M. Tierney, Jr., Eds. Ralph Gonzales, Roni Zeiger, Online Eds.
Current Medical Diagnosis & Treatment 2008
Stephen J. McPhee, Maxine A. Papadakis, and Lawrence M. Tierney, Jr., Eds. Ralph Gonzales, Roni Zeiger, Online Eds.